ServicesOverview
SERVICES OVERVIEW
Foot Care
Podiatrists are Foot Health Experts and understand the structure and movement of your feet and lower limbs.
They can assess, diagnose and treat foot, ankle, knee, leg or hip pain.
Given your feet alone house a quarter of the bones in your entire body, a podiatrist is best placed to get you moving, active or pain-free.
How Can A Podiatrist Help Me?
- Can you can only walk for a short period before your feet or legs hurt?
- Do you experience pain in your lower limbs at night?
- Do you experience tingling in your feet?
- Have you noticed your legs or feet are swollen?
- Do you have cuts or fissures on your feet that take a long time to heal?
- Are you returning to sport after an injury?
- Are you uncertain about which running or sports shoe to buy?
- Do you find that you wear out the outside of your shoes quickly?
- Have you noticed your toes poke holes in the top of your shoes?
- Does your forefoot become hot and painful after running or walking?
- Do your hips hurt?
- Has pain in your feet or legs stopped you from exercising?
- Are you worried about your child’s feet?
- Do you have arthritis in your feet?
- Do you experience reoccurring gouty attacks?
- Are you worried about the thickness of your nails?
- Do you have discoloured toe nails?
- Are you worried about your foot odour?
- Do your toe nails cause you pain?
- Have you noticed your toes are clawed?
- Do you have hard skin on your feet? Is it getting worse?
- Do you find it hard to cut your own nails?
- Do you find it hard to fit your feet into shoes because of your bunion?
Ticked one or more boxes? Then you need to see a podiatrist.

Ball Of Foot Pain

There are many types of pain from the ball of your foot, and many different reasons why they would be painful in the first place…
This condition commonly occurs with women, however many men suffer from pain in the ball of the foot. This is one of the most common causes of pain in the ball of the foot. The pain from a plantar plate injury is often exacerbated by raising onto your tip toes. This can be accompanied by swelling and also splaying of the toes or clawing toe. Plantar plate dysfunction is commonly related with bunions, traumatic or repetitive injury and wearing high-heeled shoes.
Pain located around the 3rd and 4th toes, may be associated with a neuroma (although neuromas can also occur between other toes, they occur most commonly between the 3rd and 4th toes). Neuromas can cause unusual sensations, ranging from a sharp, stabbing pain, through to a numb feeling. Often, people with a neuroma find that removing their shoes and massaging the area eases ball of foot pain.
Sesamoiditis often results from activities that put increased force on the ball of the foot, such as running or dancing. This is more common in high-arched feet. Pain is usually focused on the ball of the foot near the big toe and will often be worse when moving the big toe joint. Swelling may also be present around the base of the big toe joint.
Capsulitis is a condition where the capsular ligaments around the joint become inflamed. In the foot, capsulitis is commonly seen at the base of the second toe, although it can occur in any joint.
Corns and Calluses are very common on the ball of the foot. These thickened areas of skin are created due to increased pressure, and a corn can also develop.
Bursitis is a condition that is often secondary to other causes of ball of foot pain, and may be seen in conjunction with capsulitis, neuroma, metarsarsalgia or sesamoiditis.
Orthotics
We are leaders in the area of 3D scanning technology to create prescription bespoke Orthotic devices to suit each individual needs. Our clients tell us they love how we really listen to their problem and make a clear plan to reach their goals and become pain free and back to the activities they love.
Orthotics are custom made devices prescribed by a podiatrist to fit inside a range of your shoes. They help comfortably stabilise the foot, support the arch and help correctly align the lower limb; to assist with complaints such as foot pain, ankle and knee injuries, and flat feet. Whilst not everybody needs orthotics, for those who do, they can be a blessing giving them freedom from pain, an increase in confidence and comfort in their feet.
Orthotics are scientifically proven time and time again to be beneficial for particular foot complaints and are a fabulous tool in assisting those whose foot problems are caused by pressure, biomechanical problems, and over use of particular tendons, muscles or bones.
Using state of the art 3D scanning technology, our Podiatrists are able to provide an accurate impression of both feet. This information alongside other analytical tests, aid the podiatrist to make a bespoke orthotic for you.
Orthotics help by re-aligning your posture from the ground up. When your foot posture is incorrect the entire body structure is incorrect. Biomechanical problems can increase stresses within the foot structures and the surrounding soft tissues, creating localised pain in the feet, ankles and also problems in the lower limbs, knees, hips and back.
Foot orthotics allow the muscles, tendons and bones of the feet and lower legs to function at their highest potential by correcting misalignment. When appropriately prescribed, these orthotics can decrease pain and increase stability in an unstable joint, along with preventing potential progression or development of a deformity.


After your biomechanical evaluation, we then use a 3D scanner to create a digital image of your feet or a fibreglass model cast. Using this scan or model together with the information from your dynamic assessment our Podiatrists will design your orthotics. The design is then sent to an orthotic lab to be milled and your orthotics will be ready to pick up within 10 days. We are lucky enough to be equipped with an on-site orthotic laboratory which allows us to make any additional updates and changes to your orthotic on site as your needs change.
There are so many amazing materials available these days which means we can choose the styles and materials of your devices according to your lifestyle. Some of our favourite materials for orthotic shells include:
EVA. Using computer technology to create the right prescription for you these orthotics are perfect for people looking for a little more cushioning in their life. Like a fancy sneaker insole, these are both comfortable as well as supportive. If you get smelly feet we, on request, can also make a machine washable version of your devices.
Polypropylene. This material is the most popular material used worldwide due to its versatility and longevity. This highly versatile material is tested by time and will last for years to come.
3D Printed – With this newest and latest addition to the orthotic technology family, we are able to customize your orthotic to sub-millimetre accuracy which means they feel great. Our range of orthotics provides an extensive list of treatable conditions.
Heel Pain (Plantar Fasciitis)
Heel pain is a common and frustrating complaint affecting people from all walks of life. This pain can range in severity from a dull ache to a sharp stabbing sensation. It occurs in both children and adults, active and inactive people alike.
The most common cause of heel pain is inflammation within the plantar fascia, which is a thick fibrous band in the bottom of the foot that provides dynamic support during daily activities. There are also a number of less common conditions which may cause heel pain including nerve entrapments, heel spur, growing pains in children, stress reactions and fractures as well as injury to the fatty padding.
- Accurate diagnosis of the potential causes will require a thorough biomechanical assessment by a Podiatrist.
- Treatment and management plans are implemented based on the cause of the pain and injury. Correct diagnosis and identification of the cause will allow the best possible treatment plan to be implemented and employed, allowing you the fastest return to pain free walking.
- A number of treatment options are currently used by the team, including taping, stretching, trigger point muscle therapy, orthoses and footwear modifications.
- A holistic approach is taken when managing heel pain with the overall aim of long term prevention allowing you to function at your best.

Back Pain
It is said that up to 70% of the population will suffer from lower back pain at some stage in their lives.
There can many causes of low back pain. These may be osseous (bony), neuropathic (nerve damage) or soft tissue. One of the major causes of lower back pain is incorrect positioning of the pelvis during walking, and this is very often due to foot posture and problems with foot and leg function.
Our Podiatrists have completed extra training to enable them to examine and treat any lower limb joints and soft tissue problems as far as the pelvis and lower back muscles.
These areas must be considered when dealing with the body and its movement. This is a more holistic form of therapy as we understand that the body cannot be split into sections and must be treated as a whole.
We work very closely with your Doctor and other health professionals to help ensure your foot posture is helping and not hindering your low back pain. Call us today for a foot posture and walking analysis.
Common Causes
Abnormal pronation, or “flat feet” as they are commonly referred to, causes various rotations throughout the legs during the walking cycle. The end result of these rotations can be a forward tilt of the pelvis, which in turn increases the curvature of the spine and places strain on the muscles and ligaments of the lower back.
If one foot is rolling in or out significantly further than the other, not only is there an increased curvature through the lower back, but a pelvic tilt can result. This can lead to scoliosis ( a curvature of the spine), and once again places strain on the associated muscles and ligaments.

Treatment
This is necessary to balance the feet and control abnormal motion, thus assisting in stabilising the pelvis and enhancing the normal function of the spine.
Consulting with a chiropractor, physiotherapist or occupational therapist may also be required. This treatment will be recommended as part of your treatment program, depending on each individual’s situation.
These are often prescribed as part of your treatment program.
Your footwear is reviewed to ensure there is no aggravation of your symptoms.
Knee Pain

There are two types of injuries which can cause knee pain:
- Acute Injuries (such as ligament tears),
- Overuse Injuries (such as RSI or microtrauma).
Various factors can cause overuse injuries to the knee, including poor footwear, inappropriate training programs, and inadequate training surfaces (such as bitumen or soft sand). Another major cause is abnormal alignment of the foot and lower leg.
With flat or excessively pronated feet, the result is excessive internal rotation of the lower leg at the same time that the upper leg is rotating in the opposite direction due to forces produced during walking. The knee is the area that therefore must absorb these twisting forces, and thus injuries occur. Also, pronated feet result in a valgus, or ‘knock-knee’ position, which results in various muscles exerting their pull in incorrect directions.
High arched, or excessively supinated feet, do not allow the shock absorption needed during walking. The knee must therefore take too much force to absorb this shock, and this is when overuse injuries will occur.
Patellofemoral Syndrome. With pronated feet the knees move into the ‘knock-kneed’ position. This causes the Patellar tendon (which connects the muscles of the thigh to the lower leg via the knee cap/patella which acts as a pulley) to pull in the wrong direction. The patella thus runs over areas in the knee that it is not supposed to, and eventually this will result in injury and pain. The pain is often felt with bent-knee activity, like squatting and walking upstairs.
Iliotibial Band Syndrome. The muscle which runs down the outside of the thigh, and which crosses the knee, is the iliotibial band. With excessive pronation, this muscle shortens over time and is therefore subject to pain and injury. Pain is felt on the outer edge of the knee joint.
Osgood Shlatters Disease. This commonly affects teenagers, and is an inflammation of the growth plate of the tibia (lower leg bone), which is situated just below the kneecap.
- Orthoses, as these allow the foot, leg and knee to function in the correct position, and thus forces are distributed correctly throughout the leg.
- Exercises, that aim at strengthening and stretching of muscles around the knee.
- Anti-Inflammatory medication, rest, ice, compression.
- Physiotherapy
- Taping of the knee
- Wearing Appropriate Footwear
Laser Nail Treatment
A Revolutionary, Safe & Effective Treatment For Onychomycosis
(Fungal Infection Of Finger & Toenails)
Nail fungus is an infection in one or more of your nails. This may begin as a white or yellow spot under the tip of your fingernail or toenail. As the nail fungus spreads deeper into your nail, it may cause your nail to discolor, thicken and develop crumbling edges — an unsightly and potentially painful problem.
The best results are achieved if you are treated as soon as you discover an infection. Long standing, chronic nail infections are more resistant to treatment. An infection with nail fungus has traditionally been difficult to treat, however using the Fox laser this is no longer so. We offer a few options with regards to Laser nail therapy.
1. Initially we prepare the nails for treatment. This involves taking photos for comparison, redefining and smoothing the infected nails and providing you with all the information and education you need to maximise your chances of success.
2. The first laser treatment will treat all 10 nails at our current price of $280.
3. You will then go on to have another 2 treatments about 3 weeks apart. These subsequent treatments involve taking more photos as well as further nail preparation and then lasering of all affected nails for our current price of $180.
4. We will continue to monitor the nail health and growth with visits about 6-8 weekly. These appointments will involve more photos, comparison of photos, re-defining and cleaning up the nails, re-education where needed, and we will also make a plan for you to maintain your improved foot health. These appointments will be charged by the length of the appointment and vary from $70-$120 for 20 min to 1 hour consultations.
5. We aim for complete cure of the nail fungal infection however this is not always possible so we work hard to get your feet as healthy as they can be without having to take medications with nasty side effects.

Laser Nail Therapy Is;
- Safe
- Drug Free
- Extremely Effective
- Results In Clear Nails
If you’d like more information, please give us a call. As the most experienced podiatry clinic, in Geelong, in Laser Nail Therapy for infected nails, we’re happy to offer advice and solutions to help.
Morton's Neuroma
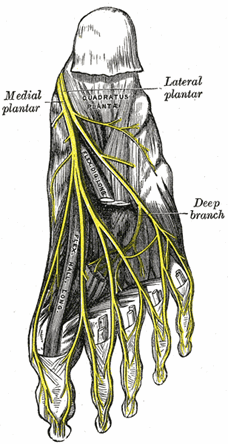
For more information, please see This paper written by M J Coughlin and T Pinsonneault, published on the National Library Of Medicine’s PubMed.
Morton’s Neuroma is a common and frustrating cause of forefoot pain within the population. The condition commonly results from a thickening or compression of the nerves between the bones of the forefoot (intermetatarsal space). This can result in a range of symptoms; from sharp pains in the ball of the foot as well as burning, numbness and other abnormal neurological symptoms that can shoot up into the toes. The cause of the pain is not currently fully understood however some suggest that it may be caused by genetics and/or long-term irritation of the nerve.
Morton’s Neuroma is typically diagnosed clinically based on the signs and symptoms and can often be assisted with imaging such as ultrasound to exclude other common causes of forefoot pain, such as bursitis, plantar plate injuries, stress fractures and/or Osteo arthritis. Treatment is focused on offloading the compression of the nerve, which can be achieved by a number of different treatments including orthotics, padding and footwear changes as well as injection therapy.
It is essential that the exact cause of the pain be identified as incorrect management options will prolong pain and, in some cases, exacerbate the severity of the injury.
The exact cause is not fully understood. A neuroma most often affects women over 50 years of age and aggravated by tight or high-heeled shoes. Faulty foot mechanics is thought to play a role. The condition seems to occur in response to irritation, pressure or injury to one of the nerves that lead to your toes. The neuroma is part of your body’s response to the irritation or injury. In some cases, Morton’s neuroma may result from abnormal movement of your foot, caused by bunions, hammertoes, flatfeet or excessive flexibility.
Pads, rest, ice, and anti-inflammatory medication can help improve comfort. Wide shoes with foot orthoses and cortisone injections may resolve the pain in some people. If the neuroma is small in size a course of 5-6 injections of local anesthetic around the neuroma can also be helpful. No long-term studies are available. However, surgery is recommended if these measures are ineffective and the problem continues to interfere with your quality of life.
The operation involves removing the enlarged nerve by a cut made on the top of the foot. The deep transverse metatarsal ligament suspected of causing some of the constriction above the nerve is released. The thickened nerve is then isolated from the surrounding tissue and cut where the nerve trunk appears normal again. An inflamed intermetatarsal bursa is often present and this is also removed. The specimen is sent for a pathology examination.
This operation (neurectomy) by a dorsal approach has shown good to excellent patient satisfaction rates (78-84%) in two good studies (1,2). The Coughlin & Pinsonneault study is a long term follow up after 11 years.
- Infection (smoking increases this risk by 16X)
- Stump neuroma can occur when little sproutlets of nerve from the cut end of the nerve starts to grow again. These sproutlets can grow into a ball that hurts like (or more than) the original neuroma and this requires further surgery to rectify.
- Wound problems (slow to heal)
- Scar sensitivity
- Nerve Injury (Nerves can be bruised which resolves but you can be left with permanent numbness)
- CRPS = Complex Regional Pain Syndrome (Rare <1%)
- Deep Vein thrombosis (clot in deep vein in the legs)
The underneath of the foot can remain tender for about 3-4 months after surgery. This is likely to resolve on its own without treatment. An orthotic will also help.
Diabetic Foot
Chronic Pain & Dysfunction
Have you ever wondered how you developed particular probems or pain? Do you repeat the same injuries or have patterns of injury such as left or right side or seem to have a weaker part of your body?
The answers may not be a complex as you think. Our Podiatrists are particularly skilled in diagnosing underlying causes present in each person, that can lead to injury or illness.
Diabetes & Associated Foot Problems
Is 4400 amputations a big enough number to make you think about foot health and diabetes.
12 people today will have a diabetes-related amputation. Tomorrow there will be 12 amputations.
85% of these amputations are preventable, as long as changes are detected early and managed effectively.
Diabetes is a lifelong condition which can create complications in the feet. Some of these issues can arise due to the nerves and blood vessels supplying the feet becoming damaged.
The peripheral nervous system is the nerves outside the central nervous system (the brain and spinal cord). There are three main types of nerves within the peripheral nervous system:
- Sensory Nerves. Provide sensations, such as pain and touch
- Motor Nerves. Controlling muscles
- Autonomic Nerves. Regulates automatic functions of the body, such as blood pressure and sweat production
- Tingling and numbness
- Burning, stabbing or shooting pain in affected areas
- Loss of balance and co-ordination
- Muscle weakness
This depends on the underlying cause and which nerves are affected.
Some cases may improve with time if the cause is addressed, whereas for some people the damage may be everlasting.
If the cause isn’t treated, you may be at risk of potentially serious complications, for instance foot ulceration may become infected.

Signs of peripheral arterial disease (PAD)
- A lot of people with PAD have no symptoms,
- Intermittent claudication: a painful ache in the legs when walking, this usually resolves after a rest,
- Weakness in the legs,
- Brittle and slow-growing toenails
- Ulcers of the feet or leg
- Skin color becoming pale or blue
- Burning pain in the legs and feet that continues with rest,
- Toes or lower limbs becoming cold and numb, developing red and then black
Changes within the feet and lower limb can happen slowly over time, and you may not detect slow changes.
At Heal and Soul Health, we recommend people with Diabetes have their feet assessed on a 6 month basis or more regularly if advised. This is in-line with the Victorian state guidelines.
- Looking at current medical history, medication and ability to self-care.
- Neurological supply to the feet: we asses all three parts of the nervous system supplying your feet to note any alteration.
- Vascular supply to and from the feet: listening to the arterial supply as well as taking a blood pressure reading in the leg and arm, to give an overall impression.
- The structure of your feet and visual gait analysis: this will aid in detecting high pressure areas which are at greater risk of ulceration.
- Ulceration and foot lesion history.
- Footwear assessment.
- Any other concerns you have
nailKALM® Cosmetic Nail Reconstruction
Bring your feet back to life with nailKALM® and enjoy younger, more healthier appearing toenails and feet. This effective anti-fungal agent, is clinically proven to provide effective treatment and restoration of damaged unsightly toenails prone to fungal infections.
- This groundbreakng treatment can assist in reducing fungal nail infections and promote healthier feet, skin and nails.
- It is 100% organic and utilises our patented non-toxic active ingredient (AMYCOT® )
- We love how gentle it is on sensitive skin, and,
- 100% Australian made


nailKALM® Information & Details
NailKALM® is not just an effective anti-fungal agent, it is THE only treatment we recommend for all ages, sensitivities and pregnancies, with consistent and highly successful clinical solutions for reducing damaged or infected toenails.
NailKALM® has also skin repair capabilities – it accelerates regeneration of keratinocytes. AMYCOT® is the active ingredient in NailKALM®.
It’s a powerful natural ingredient derived from Arthrospira maxima (Spirulina), a naturally occurring micro algae (cyanobacterium). The biosource of this product has its origin in one of the earliest forms of plant life on our planet earth. It is a microscopic, water borne, single cell plant that has been used for centuries as a highly nutritious source of food containing very high levels of essential vitamins and anti-oxidants.
The antifungal activity of AMYCOT® is due to a putative enzymatic action that destroys the chitin/chitosan polymers found in the fungal cell wall. Damage to the polymers causes the fungal walls to collapse, eventually killing the fungus.
Tests have shown NailKALM® stimulate the growth of the skin derived cells such as keratinocytes thus, enhancing skin, nail and hair growth. NailKALM® products are naturally derived, and non-sensitising.
As AMYCOT® is a plant based product there may be changes in colour and smellfrom batch to batch. This is caused by changes in the climatic conditions during the growing period. Also, should you notice that a clear liquid appears at the top of the flask, do not be concerned, the plant material absorbs water during processing and sometimes releases some of this later. If this does occur, give the tube or bottle a vigorous shake.
Although there have been no specific trials with pregnant mothers to date, there have been no reported toxicity during our clinical trials in humans and whatsoever whilst using nailKALM® until this day.
The bio-active ingredient used in nailKALM® (AMYCOT®) is 100% organic and natural, and is made from Spirulina, a microorganism, which is a popular health food and has been consumed around the world for centuries.

Pure Body

Pure Body Extra Strength’s nanosized natural zeolite is delivered in a convenient, easy-to-use spray. To provide a continuous detox to a cellular level, simply take 4 sprays, 3 times per day in the mouth, then swallow. Pure Body Extra Strength can be taken with or without food.
It starts before we’re born, and despite our body’s best efforts to remove toxins, we continue to accumulate heavy metals such as mercury, lead, arsenic and others, simply because they are everywhere.
Powdered zeolites and most detox programs only cleanse the colon. But that’s not where the majority of toxins accumulate. They’re in your cells. Pure Body Extra Strength’s zeolite uses advanced nanotechnology to reach to a cellular level for a whole-body detox.
Pure Body Extra Strength’s nanosized natural zeolite is delivered in a convenient, easy-to-use spray. To provide a continuous detox to a cellular level, simply take 4 sprays, 3 times per day in the mouth, then swallow.
Even In Small Amounts, Toxins Can...
- Store in your fat cells, making it hard to lose weight
- Mess with your memory, clarity and focus
- Interfere with your immune system
- Disrupt your endocrine system, affecting your energy
- Make it hard to fall asleep, or cause poor sleep quality
Every Serving Of Pure Body Extra Strength Works To...
- Help the body remove heavy metals and toxins*
- Support a healthy immune system*
- Help balance the body’s pH, considered essential for good health*
- Support natural energy processes*
Pure Body Extra Strength is a natural way to clean out the environmental toxins our cells fight every day.
Ingrown Toenails

Onychocryptosis (ingrown toenails) is a very painful condition, in which a spike or sharp edge of a nail has pierced and penetrated the skin surrounding the nail. It occurs most frequently in the big toe and can affect people of all age groups.
The pain is a result of the nail spike penetrating the deeper layers of the skin, and causing an acute inflammatory response. If not treated, an infection can develop which will cause pain, and swelling within the toe, and problems with fitting shoes.
There are a number of factors that may cause ingrown toenails; with faulty nail cutting and pressure from ill-fitting footwear the primary causes. Conditions that alter the appearance and shape of toenails such as thickened (Onychauxis) and fungal nail infections may also predispose to the possibility of sharp edges.
If you suspect you have an ingrown toenail or your nail is sore, it is important to have it assessed and checked by a Podiatrist. The toenail infection and swelling will not resolve spontaneously, and for this reason it must be appropriately treated. A number of different treatment options are used dependent on the stage of the ingrown toenail and the possible infection.
Treatment can range from simply removing the offending nail spike, antibiotic therapy and in some cases, a minor surgical procedure (done in the chair) to remove the nail portion permanently.
Are You Looking For Ingrown Toenail Surgery?
There are many procedures that have been developed over the years to address chronic or recurrent ingrown toenails. These range from quite invasive procedures requiring stitches and considerable change to the visual appearance of the toe and nail, to less invasive procedures with minimal post operative pain and less cosmetic effects.
At Heal & Soul Podiatry our preferred procedure for ingrown toenails is, a partial nail avulsion and matrix sterilisation (nail bed removal) done under local anaesthetic. This has been shown through research to be the most reliable form of procedure, to reduce the risk of recurrence caused by a regrowth of the nail. Nail surgery is generally very safe, with very minimal pain afterwards, and can be safely performed within our clinic.
This procedure involves removal of the outside edge of the nail, and the nail root (matrix), the cells which are responsible for nail growth, are destroyed by a chemical (phenol). It is done under a local anaesthetic toe block, which means there is no discomfort during or immediately after the procedure, and you can return home directly afterwards. Cosmetically, the nail plate will look slightly narrower once fully healed, and this is usually barely noticeable.
After the procedure, you will be sent home with the toe bandaged and instructions on what to do (pain medications, elevation, rest, keep dry, etc). Typically, your podiatrist will review you within a couple of days and change the dressing, and then given you instructions on self management of the toe (ie changing dressings yourself) over the coming 1-2 weeks. Your podiatrist will then normally review the toe as needed to make sure it is healing properly, and then follow up with you as necessary afterward.
Most people are able to return to work the day after surgery however we recommend wearing roomy shoes to prevent unecessary pressure on the toe.
Most sufferers of chronic ingrown toenails will be suitable for the procedure, however there are some situations where this may not be appropriate. This includes patients with medical conditions where there is poor circulation in the foot, certain medication treatments, or if there are other health problems your podiatrist feels may affect your ability to recover suitably from the procedure.
We understand that some people can be very worried and anxious about having minor surgery under local anaesthetic. If you are ‘needle-phobic’ or suffer from anxiety about the procedure, we are able to provide you with some options for sedation to reduce your stress and concerns. You should discuss this with your GP who may prescribe something suitable for your surgery.
Please contact us if you are worried or concerned about having injections, or the procedure in general, and talk to one of our friendly podiatrists about your options.
What Are The Benefits & Risks?
The principle benefit of ingrown toenail surgery is to provide a permanent solution to chronic pain, discomfort or infected toes. Left untreated, chronic ingrown toenails can in some circumstances lead to severe infections, affecting the toe bones and causing a deep infection known as osteomyelitis, which can be very difficult to treat.
There is a high success rate of 95% that the nail will not regrow.
No surgical procedure, no matter how large or small, is without risk.
The most common issues that may occur following ingrown toenail surgery are infection, recurrence or delayed healing. Typically, the chance of developing any of these problems with ingrown toenail surgery is very small, and measured at only a few percent of all surgical cases in healthy individuals.
Because of these potential risks, our podiatrists will discuss these issues with you, and ask that you complete a consent form to indicate you are aware of these risks before we undertake toe nail removal.
Wart Treatment

A range of treatments are available. On healthy adults, strong acid is used on persistent warts and is very effective, with usually only 3 appointments needed.
Other treatments include applying Salicylic acid which is usually painless but quite effective. Other paints and ointments may be chosen depending on what is most appropriate for the individual patient.

Plantar warts come in different varieties and can appear either individually or in clusters. The general appearance of warts resembles that of a cauliflower plant protruding from the skin.
They can appear skin-coloured making them harder to identify or covered by an overlying layer of thickened skin (callous) which adds to the discomfort when weight bearing.
Some warts can have small brown or black dots which indicates small blood supply to the overlying viral tissue.
Warts can often be confused with corns because of they both occur on the underside of the feet and exhibit similar discomfort characteristics. There are a number of distinct differences though that can rule out a wart from a corn.
- Corns hurt when direct pressure is applied to the lesion while warts may not elicit this response. Pain is reproduced however when sidewards pressure is applied to wart tissues (squeeze/pinch test).
- Warts bleed when cut while corns generally do not. This is due to the small blood supply that accompanies wart tissues.
- Removing corns usually relieves symptoms of discomfort while cutting warts may not provide complete relief from discomfort.
While the viral characteristic of warts means they can be picked up from virtually anywhere, the most common places that harbour the offending virus are damp and unsanitary places such as gym floors, swimming pools, or room floors. The virus can enter the skin through small cracks in the skin which are exposed to the virus. A person’s immune system also plays a very big role in preventing the onset of verruca infections. It is not uncommon to find that after moments of stress or illness patients have developed warts due to their immune system being suppressed. Children are more susceptible to developing warts due to their activity levels and tendency to be barefoot in environments that harbour the virus.
Warts can resolve on their own within months or years. However, whilst they are present there is a risk of them multiplying or being contagious. Plantar warts usually get deeper as they get larger, and this can become very painful to walk on. The larger and longer a wart has been present on the foot, the more difficult it becomes to treat it. So it is best to see a podiatrist for professional advice and treatment as soon as you notice a wart. Podiatrists are foot and lower limbs specialists with extensive training in the effective treatment of plantar warts. A number of treatments are available which includes:
- Sharp removal of wart tissue to reduce its physical size.
- Application of chemicals such as Nitric Acid, Silver Nitrate or Salicylic Acid to burn existing wart tissue.
- Freezing of wart tissue using liquid nitrogen
- Burning off wart tissue using a method called electrocautery
- Surgical removal of wart tissue under local anaesthetic.
- Needling of wart tissue under local anaesthetic.
- Offloading affected area to reduce discomfort during weight bearing and everyday activities.
A number of over the counter remedies are available from the chemist which may assist in eliminating the wart tissue before it becomes excessively uncomfortable. If however, over the counter remedies are deemed unsuccessful at controlling the wart, specialist assessment and advice should be sought out.
Whilst there is an element of chance in contracting warts, there are a number of methods to reduce your risk of becoming exposed to or spreading the virus. Some steps include:
- Minimising the time spent barefoot on damp floors, including gyms, communal showers and floors.
- Avoid wearing the footwear of people who have previously had or currently have plantar warts.
- Cover existing warts with waterproof plaster so that it does not contact floor surfaces.
- Wearing specialist socks during swimming activities.
- Avoid touching your or the warts of other people with your hands
- Avoid sharing towels, razors or socks with other people.
- Keep your feet as dry as possible as warts prefer moist environments.
- Avoid wearing shoes or walking on surfaces that irritate the soles of your feet as injured skin is more prone to infection.


